Experienced Back, Neck And Spinal Injury Representation
Back and neck injuries are especially debilitating for several reasons. They can cause chronic pain and muscle weakness throughout the body. If the spinal cord is injured, temporary or permanent paralysis may be the result.
Suffering a herniated disk can mean a lifetime of severe pain and additional problems. Our Fishkill law firm handles complicated musculoskeletal injury cases like these to pursue compensation on behalf of injured people. Call 845-896-5295 to schedule a free consultation with The Maurer Law Firm today.
What Is A Herniated Disc?
Disc herniation, also called a slipped disc or ruptured disc, usually occurs in the lower back (lumbar spine) or in the neck (cervical spine). It happens when an injury causes the jelly-like substance in the center of the disk to protrude through the outer ring of cartilage, putting pressure on the spinal nerves. Even minimal pressure can result in severe pain.
Sometimes the ligament that holds the disc in place between the spinal vertebrae tears, but the disc does not come out. This results in negative diagnostic testing, but the patient still experiences significant pain and disability.
This type of injury can also cause tingling, numbness, burning sensations, muscle weakness and in catastrophic cases, a loss of bladder or bowel control. Herniated discs in the lumbar region may cause pain in the sciatic nerve in the back of the leg. Injuries in the cervical spine may cause headaches as well as pain in the neck, shoulders, arms and hands. Pain and additional symptoms may prevent you from sleeping or performing daily tasks and returning to work.
Understanding The Anatomy Of The Spine
How is spine injury patient supposed to make an informed decision about his/her medical care if they don't understand the basics about the spine? The problem isn't as bad as it was a few decades ago, but many doctors still don't adequately explain the anatomy of the spine and the reasons for a patient's pain when a patient goes to an orthopedist, neurologist or neurosurgeon.
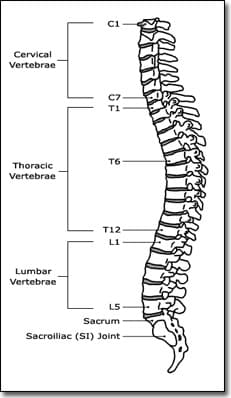
The spine is principally made up of vertebrae (bones), discs (cartilage between the vertebrae that act as shock absorbers and space maintainers), ligaments (that connect bone to bone and hold the discs in place between the bones), nerves (that convey directions to muscles to act and relay sensation to the brain) and muscles (that run up and down the spine like a pulley system).
There are seven Cervical vertebrae at the top of the spine, twelve Thoracic vertebrae in the middle of the spine, five Lumbar vertebrae in the lower spine and the Sacrum located at the bottom of the spine. The spinal cord travels down the spine and stops in the vicinity of the first Lumbar vertebra. From that point, nerves continue down. Nerve roots exit from the spine through openings called Foramina located at each level and on both sides of the spine.
Typical patient complaints include:
- Localized spine pain
- Pain, numbness and tingling radiating from the neck down one or both arms or radiating from the lower back down one or both legs
Most spinal complaints result from an injury or from arthritic degenerative changes that take place over time in all human beings. Trauma can cause damage to the discs. A "slipped" or herniated disc occurs when the trauma causes disc material to rupture through the annulus fibrosus which normally holds the disc material in place.
If the herniated disc puts pressure on the spinal cord or nerve roots that exit the cord, it can cause severe pain, numbness and tingling with radiation of the symptoms down the path of the nerve root that is being pressed upon by the herniated disc.
The role of the intervertebral discs is mechanical. They are the joints of the spine, enabling it to bend and twist in all directions. They support compressive loads arising from body weight and muscle tension and anchor one vertebral body to the next.
The discs in the human body have no blood supply and lose water content over time. If a disc thins out or bony growths (osteophytes) develop on the vertebrae, nerve roots can also be pinched as is the case with a herniated disc.
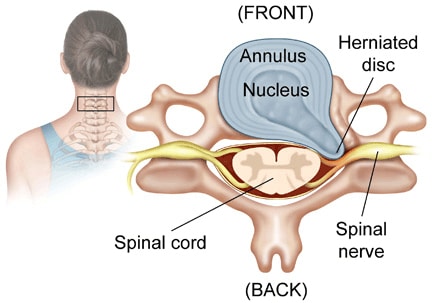
A tear in the outside of the disc (annulus fibrosus) can cause leakage of irritating fluid that results in localized disabling pain, even if the disc doesn't herniate out of its space. The torn disc will lose its normal shape and its ability to work as a shock absorber and space maintainer can be compromised.
Diagnosing Disc Herniation
Doctors have a number of methods for diagnosing the source of spine pain, numbness and tingling.
A trained orthopedist (bone surgeon) and neurosurgeon (nerve surgeon) will be able to isolate the source of a patient's spinal complaints through a combination of physical examination, diagnostics tests and by obtaining an accurate medical history from the patient. While a physical exam will yield helpful basic information, the use of modern diagnostic studies is frequently necessary if the patient's complaints appear to be the result of more than a mild sprain or strain of soft tissue.
A CT scan (computerized axial tomogram) is an X-ray procedure that combines many X-ray images with the aid of a computer to generate cross-sectional views and, if needed, three-dimensional images of the internal organs and structures of the body. A CT scan is used to define normal and abnormal structures in the body and/or assist in procedures by helping to accurately guide the placement of instruments or treatments. CT scans are generally more useful in looking at bone as opposed to soft tissue.
An MRI (magnetic resonance imaging) is a test that uses a magnetic field and pulses of radio wave energy to make pictures of organs and structures inside the body. In many cases MRI gives different information about structures in the body than can be seen with an x-ray, ultrasound, or CT scan. MRI also may show problems that cannot be seen with other imaging methods.
Pictures from an MRI scan are digital images that can be saved and stored on a computer for more study. The images also can be reviewed remotely, such as in a clinic or an operating room. In some cases, contrast dye may be used during the MRI scan to show certain structures more clearly.
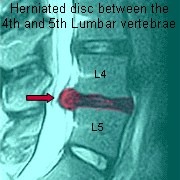
MRI testing will show most herniated discs. However, sometimes the tearing of the retaining ligament is subtle, permitting irritating, caustic fluid to leak out of the disc and causing significant pain. An MRI may not reveal this kind of damage.
Over the last 32 years, I've represented many spine injury victims with "negative" MRIs who have suffered for years with pain and restricted range of motion. In recent years, some of these victims have found help in the form of a fairly new form of testing called a provocative discogram.
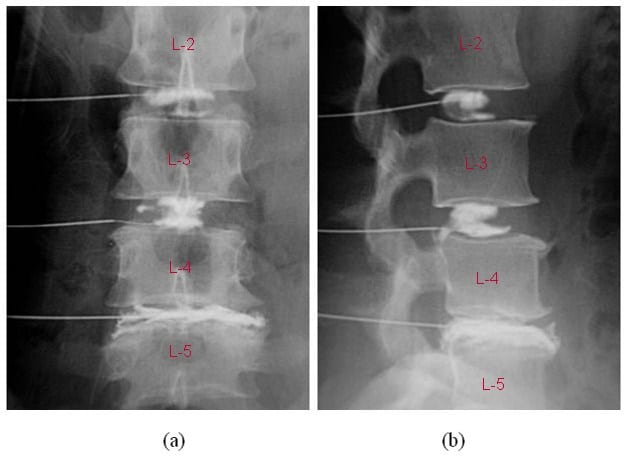
When the provocative discogram is performed, a surgeon injects dye directly into several discs and a CT scan is obtained that reveals the damaged disc is leaking the injected dye (in film (a) above, you see the dye has spread out between the L4 and L5 vertebrae). The test, performed with the patient awake, also "provokes" pain where the disc is damaged. This testing is generally performed on the lower back but not on the neck because of the risk of spinal injury from the test which could cause quadriplegia. Provocative discograms recently have fallen out of favor with some doctors.
Methods Of Treatment
Once the orthopedist or neurosurgeon has isolated the cause of the spine symptoms, they have a number of treatment paths that can be pursued. Except in the case where trauma requires immediate spine surgery, the vast majority of spine surgeons follow the same conservative approach to treatment of spine pain and other related symptoms.
After trauma to the body, there is usually swelling or inflammation of soft tissue that can compress large or small nerves and cause pain, numbness and/or tingling. Initially, application of a cold compress or ice to the injured area helps to reducing the swelling. This can be complemented by the use of an anti-inflammatory medication.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs) are medications used primarily to treat inflammation, mild to moderate pain, and fever. NSAIDs are often an effective back pain treatment option. There are many non-steroidal anti-inflammatory medications. Acetaminophen, aspirin, ibuprofen, and naproxen are the most common ones. Acetaminophen can bring down your fever, but may not work as well for conditions caused by inflammation.
Steroid anti-inflammatories are powerful medications, which are based on hormonal substances, like cortisone. These medications have a stronger anti-inflammatory response than the non-steroidal medicines. They can be taken as pills, given through your vein, or injected directly into a joint space.
Injections of epidural steroid directly into the affected joint is usually performed as a series of three separate injections. If pain is being caused by swollen soft tissue that is compressing a nerve, these kind of injections can be helpful. Steroid anti-inflammatory drugs can have powerful side effects.
Surgeons usually will employ a course of physical therapy when treating a spine injury. The physical therapy may include:
- Hot and cold therapies
- Transcutaneous nerve stimulation
- Ultrasound
- Exercise
- Massage
- Aquatic therapy in a pool
If less invasive treatments don't yield significant improvement in the patient's symptoms, there are other treatments that can be undertaken short of full-blown surgery. One approach used to treat severe chronic pain in the lower back is Radio Frequency Ablation (RFA), where radio frequency waves are used to produce heat on specifically identified nerves surrounding the facet joints on either side of the lumbar spine.
By generating heat around the nerve, its ability to transmit pain signals to the brain is destroyed. The nerves to be ablated are identified through injections of local anesthesia prior to the RFA procedure. If the local anesthesia injections provide temporary pain relief, then RFA is performed on the nerve(s) that responded well to the injections.
RFA is a minimally invasive procedure which can usually be done in day-surgery clinics, where the patient is sent home shortly after completion of the procedure. The patient is awake during the procedure, so risks associated with general anesthesia are avoided. The major drawback for this procedure is that nerves (other than the spinal cord) regenerate over time, so the pain relief achieved lasts for only a short duration (6-24 months) in most patients.
When conservative care fails and the patient is unable to live with his/her symptoms or is at risk of permanent nerve damage if untreated, surgeons will consider performing spine surgery.
In Microdiscectomy or microdecompression spine surgery, a small portion of the bone over the nerve root and/or disc material from under the nerve root is removed to relieve nerve impingement and provide more room for the nerve to heal. A microdiscectomy is typically performed for a herniated lumbar disc and is considered more effective for treating leg pain (also known as radiculopathy) than lower back pain.
A microdiscectomy is performed through a small (1 inch to 1 1/2 inch) incision in the middle of the lower back.
- First, the back muscles (erector spinae) are lifted off the bony arch (lamina) of the spine. Since these back muscles run vertically, they can be moved out of the way rather than cut.
- The surgeon is then able to enter the spine by removing a membrane over the nerve roots (ligamentum flavum), and uses either operating glasses (loupes) or an operating microscope to visualize the nerve root.
- Often, a small portion of the inside facet joint is removed both to facilitate access to the nerve root and to relieve pressure over the nerve.
- The nerve root is then gently moved to the side and the disc material is removed from under the nerve root.
- Importantly, since almost all of the joints, ligaments and muscles are left intact, a microdiscectomy does not change the mechanical structure of the patient's lower spine (lumbar spine).
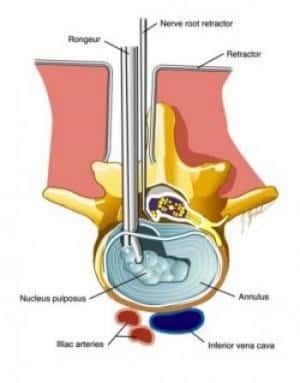
Microdiscectomy is generally performed in an otherwise healthy spine where removal of the herniated disc material is all that is required. When the spine condition is more complex and/or involves multiple levels of the spine, it is necessary for the surgeon to perform a more invasive procedure called a laminectomy.
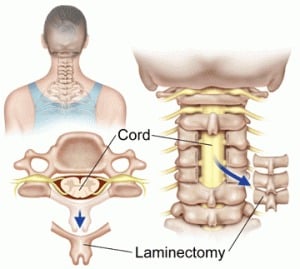
A Lumbar Laminectomy is also known as an open decompression and typically performed to alleviate pain caused by neural impingement that can result from lumbar spinal stenosis (narrowing of the spine). A condition that primarily afflicts elderly patients but can exist from birth in some patients, spinal stenosis can be caused by degenerative changes that result in enlargement of the facet joints. The enlarged joints then place pressure on the nerves, and this pressure may be effectively relieved with the laminectomy.
The lumbar laminectomy is designed to remove a small portion of the bone over the nerve root and/or disc material from under the nerve root to give the nerve root more space and a better healing environment.
The lumbar laminectomy (open decompression) differs from a microdiscectomy in that the incision is longer and there is more muscle stripping.
- First, the back is approached through a two-inch to five-inch long incision in the middle of the back, and the left and right back muscles (erector spinae) are dissected off the lamina on both sides and at multiple levels.
- After the spine is approached, the lamina is removed (laminectomy), allowing visualization of the nerve roots.
- The facet joints, which are directly over the nerve roots, may then be undercut (trimmed) to give the nerve roots more room.
Post laminectomy, patients generally remain in the hospital for one to three days, and the individual patient's mobilization (return to normal activity) is largely dependent on his/her pre-operative condition and age.
Spinal Fusion Surgery is the most invasive spine surgery procedure. Spinal fusion is designed to stop the motion at a painful vertebral segment, which in turn should decrease pain generated from the joint. There are many approaches to lumbar spinal fusion surgery, and all involve adding bone graft to an area of the spine to create a fusion, thereby stopping the motion at that segment.
Two vertebral segments need to be fused together to stop the motion at one segment, so that an L4-L5 (lumbar segment 4 and lumbar segment 5) spinal fusion is actually a one-level spinal fusion. A spine fusion surgery involves using bone graft to cause two vertebral bodies to grow together into one long bone. Bone graft can be taken from the patient's hip (autograft bone) during the spine fusion surgery, harvested from cadaver bone (allograft bone) or manufactured (synthetic bone graft substitute).
Here is what the spine looks like after the lumbar fusion surgery with the insertion of a metal rod and screws:
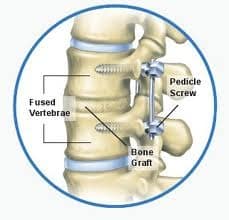
In general, a lumbar spinal fusion surgery is considered most effective for those conditions involving only one vertebral segment. A one-level spine fusion is intended to cause a limited amount of restriction in the patient's range of motion. When necessary, fusing two segments of the spine may be considered to be a reasonable option for treatment of pain. However, spinal fusion of more than two segments is reported to be less likely to provide pain relief because it limits too much of the normal motion in the lower back and places too much stress across the remaining joints.